Wednesday, October 6, 2010
Tuesday, October 5, 2010
Next Steps
At this point Bennett is doing really well. Everyone is really surprised at his great progress. So what's next?
To move from the Cardiac ICU to "the floor" he needs to be able to maintain his temperature outside of the isolette. I guess he's doing this well, because they started opening the isolette up last night, and tonight he was moved to a regular crib! He also needs to be either 2 kilos or 2.2 kilos. The doctor we spoke with yesterday couldn't remember which it was. Currently he's right around 2 kilos, but if he has to be 2.2, that means he needs to gain about half a pound.
At some point he needs to learn to take food orally. I'm not sure if that is a skill he needs to learn before he is moved or if he can learn that when he's on the floor. We attempted breastfeeding today, but he was pretty sleepy. But he got to taste some milk in his mouth. We just need to get him to learn to latch.
As an aside, in everything I've read, I've seen how pacifiers are bad for babies if you want them to breastfeed. Apparently that's not the case with preemies- especially in Bennett's case where for about two weeks now he hasn't taken any food orally. The pacifiers are good because they help them learn to suck. So I guess I have to bite my words (and the urge to throw one out today) and let him have it.
In regards to Bennett's feeding, he was being fed continuous breastmilk through a feeding tube. Today they changed it from continuous to bolus feeding. This means they are now timing it to get him used to having a full and then empty stomach. So they are feeding him every three hours, but to start off that feed took an hour and a half. When we left they had cut it back to an hour and 15 minutes, and they will continue to shorten the time it takes to feed him until they get to half hour feeds.
Once he is moved to the floor, we're almost home. He likely will only be there for a few days for us to learn how to do all of his care.
Once he is discharged, we will probably be back monthly for follow-up with the cardiologist, and depending on how he is doing, that will be changed to less frequently.
So the end is in sight. We don't know exactly how long it will be, but probably he'll be going home in the next couple of weeks. Yay, Bennett!
Sunday, October 3, 2010
An update
Here are a few updates. We've both been meaning to post with an update for quite some time now, but sitting down in front of the computer and getting our thoughts down in a coherent manner is difficult. A few days ago I started making notes to myself of things that I wanted to mention, and it just took me a few minutes to figure out what one of my notes meant. So, let's get this out before I forget even more.
Bennett milestones-
Stuff about Mumma-
Bennett milestones-
- He's started getting breastmilk via feeding tube. They tried this one day earlier in the week and had been giving him too much too soon, so they stopped and started again a couple of days later. He's now been getting it for a few days with no problems. They have added some formula to the breast milk in order to give him more calories without increasing the volume of liquid. They're hoping to help him increase his weight more quickly. Although I understand the logic behind it, I'm not sure how I feel about this. Isn't breastmilk supposed to be a superfood that shouldn't need to be supplemented?
- Earlier in the week (I don't remember which day now- Tuesday, maybe?) they turned off the meds that had been paralyzing him. It was great to slowly start to see him moving around more. First, his eyes opening, then him reacting to touching his feet, and then moving his arms. Now he's moving around like a normal little baby.
- On Wednesday he celebrated his 1 week birthday. In true scrapbooker fashion, I made a little sign for him. I plan to have these every week to begin with, then every month, as a way to show his growth.
- When I was pregnant I knit a pair of socks for him. We had brought in some other socks/booties but they've all been huge on him. The hand-knits fit perfectly! And of the nurses who come by rave about how great they are. It almost makes me want to knit another pair- except the needles that I used are so tiny it hurts to knit them.
- On Friday he had his breathing tube removed! We got to hear him cry. Such a wonderful sound.
- Thursday I got to hold him for the first time, and we've been able to hold him pretty much every day since then. Each nurse has a different way for us to hold him, and some like him piled up with blankets more than others, but it's great to be able to do this. I just wish I had asked earlier. We had kind of thought we weren't allowed since there were so many tubes/wires. I asked one of the nurses on Thursday when I would be able to, and she seemed shocked that I hadn't held him yet. She quickly made sure that I was able to do so.
Stuff about Mumma-
- Pumping has gotten much better! There are some better days than others, but overall it's going well. Monday one of the lactation consultants came by. She spent about half an hour with me, massaging and squeezing my breasts to work out the clogged ducts. We got 150ML out of me, compared to maybe the 15-30 I had been getting on my own. Wow! I haven't gotten nearly that much since, but it's been going well. And when I start to have problems I know how to fix them. And she's come back frequently since then and helps me with little problems I'm having. Chris and I kid around that Kim is my new best friend. :) I was having some problems with my pump yesterday, but Chris and I came up with a work-around. We'll need to ask Kim if it's a problem with the pump or if it was something with me- maybe another clog or something.
- After the struggles that I was having with pumping, the nurse tonight commented that I have so much milk at the hospital now that I don't need to bring in what I pump at home- we can just freeze it and keep it for ourselves. I guess it's nice to know I'm already building up a stash. Apparently I'm a very good producer and I have no issues with my supply. She also suggested that since I have such a good supply I shouldn't set an alarm at night and that I should let myself sleep, but I disagree with that advice.
- When I was over at the Brigham, the nurses were constantly checking my feet to see if they were swollen. They never really got that bad. Monday they were very swollen. Tuesday they were just as bad. Wednesday I went over to my OB's office to follow up on some paperwork and asked if a nurse could take a look at my feet. They brought me back and had me do the normal OB appointment stuff- blood pressure check, weight check, and urine check. Odd just for swollen feet, but whatever. Apparently my blood pressure was rather high. 20 minutes later they re-checked and it was fine. But since it was high my OB freaked out. No one ever looked at my feet, but she sent me off to have some blood work done and to come back the next day for another BP check. She also wrote me a script for a diuretic in case I was retaining extra fluid. By the time I got home, without taking any pills, my feet were much better. The next day, my blood pressure was fine. This OB likes to worry about everything!
- One nice thing about going back to the OB was that because of the weight check, I was able to see how much I've lost. But the results surprised me. On Wednesday, a week after giving birth, I had only lost 5 pounds. That's not much more than Bennett weighs. We had just eaten, so that may have accounted for some of it. By Thursday's appointment I was down another 2 pounds, so I imagine a lot of it was food/water weight.
Wednesday, September 29, 2010
He has a new talent!
I know it's not the most exciting video, but after spending a week not seeing this, those blinks were amazing! (Ignore the chatter in the background.)
Week One: September 22nd - 29th
Tuesday, September 28, 2010
Medical Update
Daddy Chris here to give you an update on all that has happened to Bennett over the last week (because somehow I've managed to remember most things that have happened).
When Bennett was born Wednesday night the doctors and nurses in the Brigham NICU were very pleasantly surprised with how pink he was and how good his blood oxygen levels were given the severity of his heart defect. They did all the normal things for a new baby-weighed him, put the ointment on his eyes, etc. During the time that they were doing their thing a cardiologist from Children's was talking to me about the heart defect that Bennett had. None of what he told me was new, but it served to make me focus on what he was saying instead of worrying about what the others were doing.
Once they got through there checklist he was moved over to Children's. Chris and I had discussed earlier in the evening about whether they would use the same bridge that everyone uses or if there was some other way to transfer patients. Turns out they use the same bridge. On the way over the bridge the cardiologist from Children's pressed his ID badge against the card reader and the door opened. While we waited for the rest of the caravan I asked him how I was supposed to get back to the Brigham. He looked at me kinda funny and I said
"You used your ID to open the door. I don't have an ID that opens the door. How do I get back?"
Pauses...."I don't know. Maybe the ICU nurses will know how to do that."
Let me just say now, the CICU nurses at Children's are the greatest. From the time I walked into Bennett's room there was a nurse there explaining exactly what they were doing, making sure the 3-4 doctor's who came in knew that I was the Dad, made sure everyone knew that he had a name and what it was, and was so calm about it that I just relaxed. The Brigham NICU people seemed to be in a rush. All of the Children's doctors and nurses seemed very calm. Each doctor that came in the room took a few minutes to introduce themselves and chat with me before leaving again. Liz, the nurse that was with Bennett his first night was great. She explained everything that the others were doing and when the commotion had died down took the time to explain what all the numbers on the screen meant and what they should be, what the next steps were going to be, and then very politely said he was in for a long night and I should probably go see how Chris was doing. She then found a security guard to escort be back across the bridge to the Brigham.
At 4am Thursday morning, the phone rings. They are going to put Bennett on some drugs that will make him paralyzed and painless. I asked something to the effect of should we come over and he told me that there would be a lot of people in the room. We discovered this is polite doctor speak for "don't come over here right now." When we went to see Bennett later that day he was completely immobile and had many tubes and wires all over his little body. The doctor came in and said that they were going to have to do surgery as soon as the surgeon finished with his current operation.
This is when the people started showing up. The anesthesiologist showed up to explain what they were going to do and then we had to sign the consent forms. Later a second anesthesiologist came in and said the same things. Then the cardiologist came in and explained briefly what they were going to try. Later the surgeon came in when he had finished his other surgery and explained exactly what he was going to do. He told us that they were going to try tying off the ductus arteriosus and seeing if that worked before permanently closing the ductus. He said once they tied it off they may have to wait 2-3 hours before they could determine if it worked. This would mean that Bennett was on the table just being watched. If that didn't work they would attempt to separate the tricuspid valve from the wall of the heart and possibly repair or replace the pulmonary valve. All this was expected to take at minimum 6 hours. Then the nurses started coming in and re-explaining everything. Somehow the two of us held it together.
At 1o'clock they were ready to take Bennett down for surgery. We were offered the chance to kiss him and hug him. Up to this point we didn't know that we could kiss him, so we both declined. When they wheeled him out of the room, I started crying. We stayed around for about another 10 minutes and then made our way back to the Brigham to wait.
At 3:20 I received a call saying they had made the first incision at 3o'clock. The next call would be when he went on the heart bypass machine. I went to take care of some paperwork at Children's and missed a call from the surgeon. At 4o'clock they had finished the surgery. Closing off the ductus had had such an immediate effect that they didn't need to try anything else at that time. Later that evening we went to see him. This was when the anesthesiologist told us that he had the most lines in the hospital. The cardiologist came by to visit and tell us how the surgery went. For the time being his lungs were getting the blood they needed. It wasn't flowing in the proper way, but it was getting there. We stayed for a little while longer that night. The nurse told us that the first 12 hours after heart surgery are the most critical, with the 12th hour being the absolute most critical. This timeline made 4:30am the critical hour.
The next morning I woke with a start, looked at the clock and realized it was 6am. I looked at my phone and realized no one had called. The critical hour had come and gone with no phone call. I called my parents who were driving up from Georgia and told them the good news. When we arrived at his room that morning the nurse told us that he had had a very uneventful night. His blood pressure dipped around 3am but obviously not enough to warrant a call. He had made it past a very critical stage.
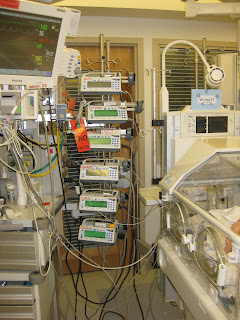
The next few days saw lots of little changes. He was very swollen from the surgery and the extra fluids they were pumping into his body. However, he was peeing like a champ which was helping to get rid of the fluid. As part of the surgery they hadn't closed his chest. They put a green membrane over the opening that was sutured to the surrounding skin. This allowed room for the impending swelling and gave them quick access if something should go wrong. Before the surgery they offered to show us another baby in the unit with a similar membrane, so that we wouldn't be shocked when he came back. We said no. We could have seen a hundred babies that had had their chests opened this way and it wouldn't have prepared us for seeing OUR son with his chest open like that. At this point he had at least a dozen pumps that were giving him controlled doses of medicine.
Saturday saw him with a few less pumps and lines. Sunday was a status quo day. At some point we brought in a blanket and Paddington Bear to put in his bed. We started adopting the policy that no news is good news. When we arrived in the morning the nurses would give us a very thorough update of how Bennett had done overnight and what was expected of him for the day to come.
On Monday we decided to run some errands on our way to the hospital, so we got there a little later than normal, probably around 1 or so. Chris had to go pump again. I feel bad because whenever we're there, she has to spend so much time pumping and I get to spend time with Bennett. I know this will change once he comes home and I go back to work, but right now I feel a little guilty that I get more time with him. I've also discovered that I really only talk to him when there is no one else in the room. These are mainly lectures on how he really has no choice in the matter, he's going to get better. We brought a book from Chris' Shower to read to him but didn't get the chance. I picked "The Little Engine That Could."
While Chris was away pumping on Monday, the cardiologist came in said they were going to close up Bennett's chest. They felt he had done well and saw no reason to leave it open longer. Within the hour they would come in and close him up. This was at 2pm. By 5pm they were just getting ready to sew him shut. We stayed until a little after 5pm and then headed home for my birthday dinner that my dad was preparing. Again, no news is good news. At 8pm that night I called to find out how Bennett had done, the nurse told us that everything had gone perfectly. They didn't even have to adjust his meds, and his blood pressure was nice and steady, which was a major concern. Quite possibly the best birthday present I will ever receive.
When we went in to see him this morning, the first thing we both noticed was that we could see a lot more of him. Overnight he had lost quite a few of his lines. And his hands were now visible since both IVs had been removed. We were also told that they had stopped the medication that was making him immobile. This drug takes quite a while to get out of his system, but it meant he would start to open his eyes and maybe move a bit. We were happy to touch his new found hands. After he had his diaper changed we put on some socks that we brought from home. They go pretty much to his knees. And we put a hat on him. I was so scared to move his head that the nurse had to lift up his head so that I could put the hat on. Again, the hat is way to big for him and it was the smallest we had. Around 1pm Kelly showed up and we went to look at Bennett again. I noticed that his eyes were open a little wider than before. As Chris went to get the camera, he closed them. We got very excited that he was opening his eyes. We stared at him for quite a while as he tried to open and close his heavy eyelids. For Chris, who hadn't seen him move at all, this was wonderful. Later when Uncle Andrew and Aunt Gentry stopped by, Bennett entertained us by opening his eyes very wide and then closing them again. I put my finger in to hold his hand and two of his fingers twitched. The paralytic was starting to wear off. Hopefully tomorrow he'll be more responsive. They also stopped his Fentinol, which is his pain medication. So from Friday having a dozen pumps, he now only has 4, and one of those is his Lipids (yum, fat).
So now it's all about meeting goals. He needs to be weened off the Nitrous Oxide which is helping his lungs, the breather which is breathing for him (this was needed while he was paralyzed, but should be less needed as he becomes more active), and start taking breastmilk through a feeding tube, ultimately moving to at least a bottle if not breastfeeding. Once he does all of these things he may be allowed to leave the Cardiac ICU and go to another wing on the same floor. But leaving the CICU is one step closer to coming home. He will need more surgeries to fix his heart fully, but the doctors hope that it will be months, years or even a decade before they have to do that surgery. But they just don't know. The longer he is out of the hospital and growing, the greater their chance of success with later surgeries.
The nurses have told us from the beginning that they are the most expensive babysitters Bennett will ever have. I would gladly pay every penny the day he comes home.
When Bennett was born Wednesday night the doctors and nurses in the Brigham NICU were very pleasantly surprised with how pink he was and how good his blood oxygen levels were given the severity of his heart defect. They did all the normal things for a new baby-weighed him, put the ointment on his eyes, etc. During the time that they were doing their thing a cardiologist from Children's was talking to me about the heart defect that Bennett had. None of what he told me was new, but it served to make me focus on what he was saying instead of worrying about what the others were doing.
Once they got through there checklist he was moved over to Children's. Chris and I had discussed earlier in the evening about whether they would use the same bridge that everyone uses or if there was some other way to transfer patients. Turns out they use the same bridge. On the way over the bridge the cardiologist from Children's pressed his ID badge against the card reader and the door opened. While we waited for the rest of the caravan I asked him how I was supposed to get back to the Brigham. He looked at me kinda funny and I said
"You used your ID to open the door. I don't have an ID that opens the door. How do I get back?"
Pauses...."I don't know. Maybe the ICU nurses will know how to do that."
Let me just say now, the CICU nurses at Children's are the greatest. From the time I walked into Bennett's room there was a nurse there explaining exactly what they were doing, making sure the 3-4 doctor's who came in knew that I was the Dad, made sure everyone knew that he had a name and what it was, and was so calm about it that I just relaxed. The Brigham NICU people seemed to be in a rush. All of the Children's doctors and nurses seemed very calm. Each doctor that came in the room took a few minutes to introduce themselves and chat with me before leaving again. Liz, the nurse that was with Bennett his first night was great. She explained everything that the others were doing and when the commotion had died down took the time to explain what all the numbers on the screen meant and what they should be, what the next steps were going to be, and then very politely said he was in for a long night and I should probably go see how Chris was doing. She then found a security guard to escort be back across the bridge to the Brigham.
At 4am Thursday morning, the phone rings. They are going to put Bennett on some drugs that will make him paralyzed and painless. I asked something to the effect of should we come over and he told me that there would be a lot of people in the room. We discovered this is polite doctor speak for "don't come over here right now." When we went to see Bennett later that day he was completely immobile and had many tubes and wires all over his little body. The doctor came in and said that they were going to have to do surgery as soon as the surgeon finished with his current operation.
This is when the people started showing up. The anesthesiologist showed up to explain what they were going to do and then we had to sign the consent forms. Later a second anesthesiologist came in and said the same things. Then the cardiologist came in and explained briefly what they were going to try. Later the surgeon came in when he had finished his other surgery and explained exactly what he was going to do. He told us that they were going to try tying off the ductus arteriosus and seeing if that worked before permanently closing the ductus. He said once they tied it off they may have to wait 2-3 hours before they could determine if it worked. This would mean that Bennett was on the table just being watched. If that didn't work they would attempt to separate the tricuspid valve from the wall of the heart and possibly repair or replace the pulmonary valve. All this was expected to take at minimum 6 hours. Then the nurses started coming in and re-explaining everything. Somehow the two of us held it together.
At 1o'clock they were ready to take Bennett down for surgery. We were offered the chance to kiss him and hug him. Up to this point we didn't know that we could kiss him, so we both declined. When they wheeled him out of the room, I started crying. We stayed around for about another 10 minutes and then made our way back to the Brigham to wait.
At 3:20 I received a call saying they had made the first incision at 3o'clock. The next call would be when he went on the heart bypass machine. I went to take care of some paperwork at Children's and missed a call from the surgeon. At 4o'clock they had finished the surgery. Closing off the ductus had had such an immediate effect that they didn't need to try anything else at that time. Later that evening we went to see him. This was when the anesthesiologist told us that he had the most lines in the hospital. The cardiologist came by to visit and tell us how the surgery went. For the time being his lungs were getting the blood they needed. It wasn't flowing in the proper way, but it was getting there. We stayed for a little while longer that night. The nurse told us that the first 12 hours after heart surgery are the most critical, with the 12th hour being the absolute most critical. This timeline made 4:30am the critical hour.
The next morning I woke with a start, looked at the clock and realized it was 6am. I looked at my phone and realized no one had called. The critical hour had come and gone with no phone call. I called my parents who were driving up from Georgia and told them the good news. When we arrived at his room that morning the nurse told us that he had had a very uneventful night. His blood pressure dipped around 3am but obviously not enough to warrant a call. He had made it past a very critical stage.
The next few days saw lots of little changes. He was very swollen from the surgery and the extra fluids they were pumping into his body. However, he was peeing like a champ which was helping to get rid of the fluid. As part of the surgery they hadn't closed his chest. They put a green membrane over the opening that was sutured to the surrounding skin. This allowed room for the impending swelling and gave them quick access if something should go wrong. Before the surgery they offered to show us another baby in the unit with a similar membrane, so that we wouldn't be shocked when he came back. We said no. We could have seen a hundred babies that had had their chests opened this way and it wouldn't have prepared us for seeing OUR son with his chest open like that. At this point he had at least a dozen pumps that were giving him controlled doses of medicine.
Saturday saw him with a few less pumps and lines. Sunday was a status quo day. At some point we brought in a blanket and Paddington Bear to put in his bed. We started adopting the policy that no news is good news. When we arrived in the morning the nurses would give us a very thorough update of how Bennett had done overnight and what was expected of him for the day to come.
On Monday we decided to run some errands on our way to the hospital, so we got there a little later than normal, probably around 1 or so. Chris had to go pump again. I feel bad because whenever we're there, she has to spend so much time pumping and I get to spend time with Bennett. I know this will change once he comes home and I go back to work, but right now I feel a little guilty that I get more time with him. I've also discovered that I really only talk to him when there is no one else in the room. These are mainly lectures on how he really has no choice in the matter, he's going to get better. We brought a book from Chris' Shower to read to him but didn't get the chance. I picked "The Little Engine That Could."
While Chris was away pumping on Monday, the cardiologist came in said they were going to close up Bennett's chest. They felt he had done well and saw no reason to leave it open longer. Within the hour they would come in and close him up. This was at 2pm. By 5pm they were just getting ready to sew him shut. We stayed until a little after 5pm and then headed home for my birthday dinner that my dad was preparing. Again, no news is good news. At 8pm that night I called to find out how Bennett had done, the nurse told us that everything had gone perfectly. They didn't even have to adjust his meds, and his blood pressure was nice and steady, which was a major concern. Quite possibly the best birthday present I will ever receive.
When we went in to see him this morning, the first thing we both noticed was that we could see a lot more of him. Overnight he had lost quite a few of his lines. And his hands were now visible since both IVs had been removed. We were also told that they had stopped the medication that was making him immobile. This drug takes quite a while to get out of his system, but it meant he would start to open his eyes and maybe move a bit. We were happy to touch his new found hands. After he had his diaper changed we put on some socks that we brought from home. They go pretty much to his knees. And we put a hat on him. I was so scared to move his head that the nurse had to lift up his head so that I could put the hat on. Again, the hat is way to big for him and it was the smallest we had. Around 1pm Kelly showed up and we went to look at Bennett again. I noticed that his eyes were open a little wider than before. As Chris went to get the camera, he closed them. We got very excited that he was opening his eyes. We stared at him for quite a while as he tried to open and close his heavy eyelids. For Chris, who hadn't seen him move at all, this was wonderful. Later when Uncle Andrew and Aunt Gentry stopped by, Bennett entertained us by opening his eyes very wide and then closing them again. I put my finger in to hold his hand and two of his fingers twitched. The paralytic was starting to wear off. Hopefully tomorrow he'll be more responsive. They also stopped his Fentinol, which is his pain medication. So from Friday having a dozen pumps, he now only has 4, and one of those is his Lipids (yum, fat).
So now it's all about meeting goals. He needs to be weened off the Nitrous Oxide which is helping his lungs, the breather which is breathing for him (this was needed while he was paralyzed, but should be less needed as he becomes more active), and start taking breastmilk through a feeding tube, ultimately moving to at least a bottle if not breastfeeding. Once he does all of these things he may be allowed to leave the Cardiac ICU and go to another wing on the same floor. But leaving the CICU is one step closer to coming home. He will need more surgeries to fix his heart fully, but the doctors hope that it will be months, years or even a decade before they have to do that surgery. But they just don't know. The longer he is out of the hospital and growing, the greater their chance of success with later surgeries.
The nurses have told us from the beginning that they are the most expensive babysitters Bennett will ever have. I would gladly pay every penny the day he comes home.
Subscribe to:
Comments (Atom)